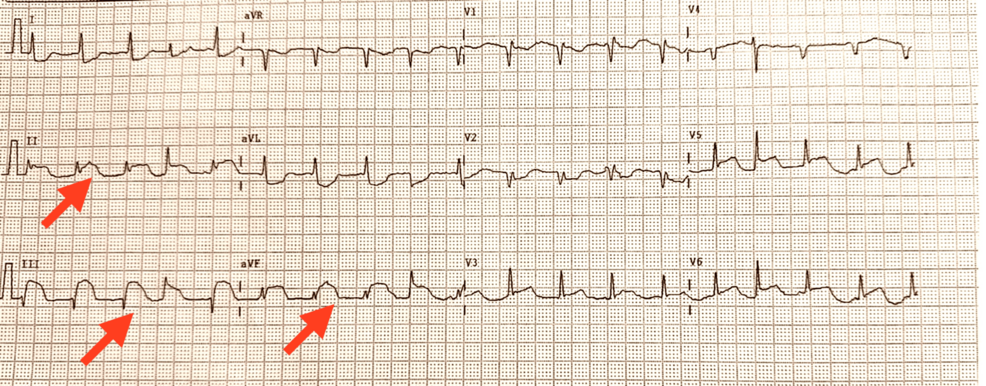
In patients presenting with chest pain and ST-segment elevations on ECG, clinicians often proceed as if a heart attack is underway. Over the past decade, however, clinicians have documented cases in which inflammatory heart disease—myocarditis—driven by infection, including sepsis, produced a clinical picture that mimics acute coronary syndromes, sometimes with inferior ST elevations. These presentations underscore a critical diagnostic challenge for frontline providers caring for acutely ill patients. ([pubmed.ncbi.nlm.nih.gov](https://pubmed.ncbi.nlm.nih.gov/38021557/?utm_source=openai))
Myocarditis is inflammation of the heart muscle that can follow a viral or bacterial infection. In some septic patients, the heart’s response resembles an acute coronary syndrome on ECG, with troponin elevations, but without a detectable blockage in the major coronary arteries. In several reported cases, coronary angiography shows non-obstructive arteries, and subsequent imaging with cardiac magnetic resonance (CMR) or, less commonly, biopsy confirms myocarditis. This distinction matters because management shifts from standard revascularization strategies to treating the infection and supporting the heart’s function. ([nhlbi.nih.gov](https://www.nhlbi.nih.gov/health/heart-inflammation/myocarditis?utm_source=openai))
Study Findings
Across case reports and reviews, clinicians note that myocarditis can present with chest pain, elevated troponin, and ST-segment changes that resemble STEMI, yet angiography reveals clean coronaries. Cardiac MRI often provides key evidence: edema and non-ischemic patterns of late gadolinium enhancement that differ from typical infarction. The National Heart, Lung, and Blood Institute (NHLBI) emphasizes a diagnostic approach based on ECG findings, biomarkers, echocardiography, MRI, and, rarely, endomyocardial biopsy when the diagnosis remains uncertain. These imaging and test combinations help distinguish inflammatory injury from obstructive coronary disease and guide appropriate treatment. ([pubmed.ncbi.nlm.nih.gov](https://pubmed.ncbi.nlm.nih.gov/38021557/?utm_source=openai))
Beyond isolated myocarditis, clinicians increasingly recognize sepsis-induced myocardial dysfunction as a related, distinct phenomenon. Sepsis-related cardiac changes can be heterogeneous: some patients exhibit depressed systolic function; others show preserved or even supranormal function, and several imaging modalities reveal diastolic dysfunction or right-ventricular involvement. Most reviews describe sepsis-induced cardiomyopathy as a reversible condition that commonly improves within 7–10 days, provided the underlying infection and hemodynamic instability are managed effectively. This dynamic underscores why careful diagnostic discrimination is essential in the critical-care setting. ([jintensivecare.biomedcentral.com](https://jintensivecare.biomedcentral.com/articles/10.1186/s40560-015-0112-5?utm_source=openai))
Expert Commentary
Experts stress that infection-related cardiac inflammation sits on a spectrum that includes myocarditis and septic cardiomyopathy. While traditional STEMI protocols emphasize rapid revascularization, a sizeable body of opinion in critical care and cardiology recommends tailoring therapy to the underlying cause when obstructive coronary disease is absent. Rapidly addressing the infection, optimizing perfusion, and avoiding unnecessary invasive procedures can improve outcomes for patients with inflammatory cardiac involvement. These perspectives are reflected in comprehensive reviews of sepsis-induced cardiomyopathy and in patient information from major health institutes that outline diagnostic pathways and management priorities. ([jintensivecare.biomedcentral.com](https://jintensivecare.biomedcentral.com/articles/10.1186/s40560-015-0112-5?utm_source=openai))
Public Health Implications
The recognition that infection-driven myocardial inflammation can masquerade as STEMI has tangible public-health significance. Misdiagnosis can expose patients to unnecessary procedures such as thrombolysis or coronary angiography with potential complications, while delaying the initiation of targeted antimicrobial or antiviral therapy and appropriate sepsis management. In septic patients, maintaining hemodynamic stability—through fluids, vasopressors, and careful use of inotropes—takes precedence, with imaging guiding subsequent decisions. For clinicians and health systems, this underscores the value of access to advanced cardiac imaging (such as CMR) and multidisciplinary collaboration in the emergency and ICU settings. ([pubmed.ncbi.nlm.nih.gov](https://pubmed.ncbi.nlm.nih.gov/16878641/?utm_source=openai))
Public-health-minded readers should note that myocarditis can arise from multiple causes, including vaccines and infections, and organizations such as the NHLBI and the American Heart Association provide ongoing guidance for clinicians and patients on recognizing symptoms, pursuing appropriate testing, and understanding prognosis. Although most myocarditis cases are rare and often self-limiting, some infections can lead to longer-term cardiac changes, reinforcing the need for follow-up care after a septic illness. ([nhlbi.nih.gov](https://www.nhlbi.nih.gov/health/heart-inflammation/myocarditis?utm_source=openai))
Next Steps in Research
Researchers continue to push for clearer definitions and diagnostic criteria for septic cardiomyopathy and infection-related myocarditis. A 2023 landscape review and subsequent studies highlight substantial heterogeneity in reported prevalence and imaging findings, underscoring the need for standardized diagnostic pathways and multi-center trials to guide therapy. Emerging data from cardiovascular magnetic resonance and advanced echocardiography, including strain imaging, are helping to delineate inflammatory cardiac injury from ischemic disease and may enable more precise prognostication for sepsis survivors. The trajectory of this work emphasizes integrating infectious disease care with cardiovascular monitoring to improve outcomes in patients with severe infections. ([academic.oup.com](https://academic.oup.com/eurheartj/article/44/Supplement_2/ehad655.1107/7392451?utm_source=openai))
In the broader context of sepsis survivorship, studies using advanced imaging suggest lasting cardiac changes in a subset of patients, which may inform follow-up strategies and rehabilitation. This area remains an active field of inquiry, with potential implications for long-term cardiovascular risk reduction and quality of life after severe infection. ([mdpi.com](https://www.mdpi.com/2075-4418/15/8/997?utm_source=openai))
For clinicians seeking context and practical guidance, authoritative summaries emphasize that myocarditis and septic cardiomyopathy are complex, dynamic conditions that require a nuanced diagnostic approach and a focus on treating the underlying infection and supporting the patient’s hemodynamics. Read more on Globally Pulse Health about how inflammatory heart disease can intersect with infectious diseases, and how clinicians balance diagnostic precision with urgent patient needs. Read more on Globally Pulse Health.
External context: for readers seeking reputable background, the National Heart, Lung, and Blood Institute (NHLBI) provides patient-centered information on myocarditis, including causes, diagnostic tests, and treatment considerations, while major health organizations emphasize the role of imaging like MRI in diagnosing inflammatory heart disease. NHLBI: Myocarditis, American Heart Association: Myocarditis.
Why this matters: recognizing infection-related myocardial inflammation early informs both infection control and cardiovascular care, helping to avoid unnecessary invasive procedures and ensuring timely treatment of the underlying illness, which can improve short-term and longer-term outcomes for patients who experience severe infections. ([nhlbi.nih.gov](https://www.nhlbi.nih.gov/health/heart-inflammation/myocarditis?utm_source=openai))